
Maheswar Rao, M.D., AGAF, FACG
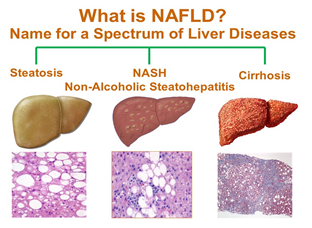
NAFLD refers to accumulation of fat in the liver cells that is not caused by alcohol. NAFLD is recognized as the most common chronic liver disease in the western world. More than 35% of US population 35-65 years old have NAFLD(more than 55 million Americans), 15 folds higher than hepatitis C (HCV). Progression of excessive liver fat will lead to non-alcoholic steatohepatitis (NASH). NASH causes liver swelling and damage, which may advance to cirrhosis, liver failure and cancer.
Primary NAFLD is more common and associated with insulin resistant state like diabetes, obesity, dyslipidemia, and metabolic syndrome. Secondary NAFLD, is less common, caused by malnutrition, drugs, metabolic disease, infections and toxins.
NAFLD is usually asymptomatic. Rarely patient may have fatigue or discomfort in the upper abdomen. Symptoms of NASH and advanced cirrhosis include abdomen swelling/fluid build up, enlarged liver/spleen, red palms, and yellow jaundice of eyes and skin.
Complications of progressive liver disease/cirrhosis vary from fluid in abdomen(ascites), swelling of vein in esophagus and stomach(varies), confusion, drowsiness, slurred speech(encephalopathy), liver cancer and end stage liver failure.
Diagnosis of NAFLD/NASH is based on blood tests: liver enzymes, liver function test, hemoglobin A1C, blood cholesterol, and triglycerides. UltrasonographyUS), computed tomography(CT), MRI, Transient Elastography(measure liver stiffness), MR elastography(MRE), Fibrotest and Fibrosure can be used to non invasively diagnose NAFLD.
No medicine have been approved to treat NAFLD/NASH. Few drugs have been studied with minimal benefits. That include: metformin, pioglitazone, rosiglitazone, vitamin E & C, betaine, taurine, N-Acetyl cysteine, sibilin, UDCA, statins, orlistat, fibrate, phentermine, anti-TNF, pentoxifylline, and antifibrotic medications.
Hence prevention of NAFLD/NASH should aimed at preventing the development of insulin resistance and its clinical manifestations (i.e, metabolic syndrome). Several useful steps have been recommended:
- Choose healthy plant based diet
- Maintain healthy body weight (BMI 20 -25)
- Regular exercise: > 5 hours(260 to 300 minutes) per week
- Calorie restriction and portion control of your meal
- Eliminate or significantly reduce saturated fats and fructose in the diet
- Good control of diabetes is essential
- Vitamin E 400 or 800 IU once daily improves histology in non diabetic NASH patients. Not effective in diabetic with NASH
- Metformin and statins improve metabolic parameters but no direct improvement in NAFLD/NASH
- In severe metabolic syndrome and obesity (BMI >35) weight surgery improves histology in NASH up to 80% cases. But consideration of bariatric surgery in presence of cirrhosis warrant careful deliberation to ensure the best outcomes.
- Urban Indian healthy male have a high prevalence of NAFLD.
- Ask your doctor to screen for NAFLD/NASH if you have: BMI > 25, waist circumference > 36” (male), >32” (female), systolic blood pressure > 130 mmHg, diastolic blood pressure > 80 mmHg, elevated fasting blood sugar > 100 mg/dL, hemoglobin A1C (HgbA1C) > 6%, triglyceride > 150 mg/dL or reduced HDL cholesterol < 40 mg/dL (male) and < 50 mg/dL (females).
- Minimize drinking alcohol and OTC medications.

Leave a Reply